The most common ophthalmic procedure that is performed is an intravitreal injection with more than 10 million per year in the USA. These injections of anti-VEGF and corticosteroid medications are helpful in treating retinal disease and inflammation. For the vast majority of patients, these intravitreal injections are easy, painless, and beneficial, however there can be rare complications such as infection. Another potential complication is iatrogenic damage to the crystalline lens capsule during the injection.
During the cataract consultation patients with a history of prior intravitreal injections should have a careful examination of the posterior capsule, using the red reflex of retro-illumination to highlight any defects or opacities. Penetration of the lens capsule by an intravitreal injection will cause either a total white cataract due to liquefaction of the cortex or a small focal defect like we see here. A history of developing a total white cataract within a week or two of an intravitreal injection is very suspicious for extensive posterior capsule damage.
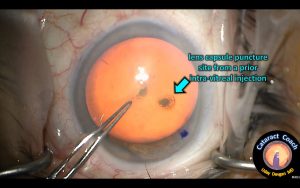
This patient had multiple prior intravitreal injections for macular disease and now presents for cataract surgery. Upon examination, there is moderate nuclear sclerosis and another small, focal lens opacity (figure 1). This is the site where the needle penetrated the lens capsule. Cataract surgery in this case will be very high risk since the posterior capsule has this weak spot which will easily break. The cataract lens material may fall into the vitreous cavity and require a pars plana vitrectomy surgery as well.
The best approach to this case is to treat it like a posterior polar case. This means avoiding hydro-dissection because that will cause pressure which will blow out the posterior capsule. Instead, do just hydro-delineation and remove the lens endo-nucleus, then use a dispersive visco-elastic to perform visco-dissection. This slow wave of dispersive visco-elastic will slowly dissect the epi-nucleus and cortex from the capsule and will tamponade any break in the posterior capsule.
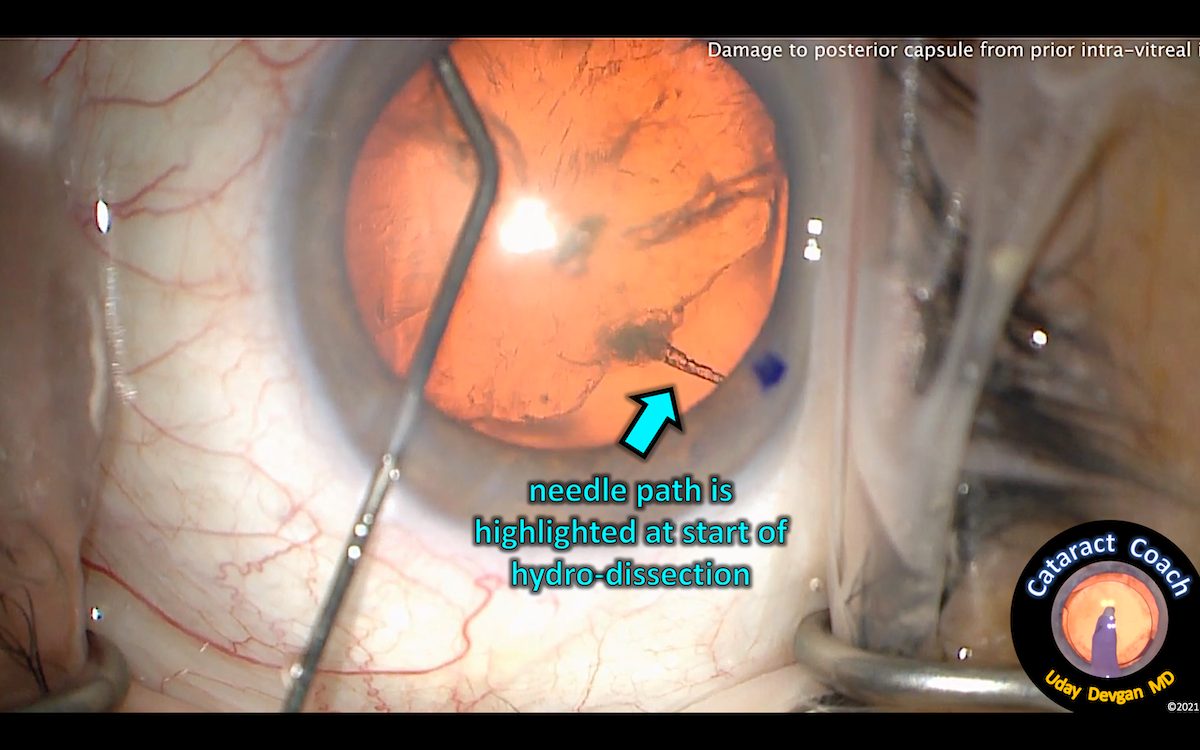
In the case shown here, standard hydro-dissection was performed and this immediately reveals the needle tract within the crystalline lens (figure 2). This happens so quickly that it is easy to miss. Continued hydro-dissection pressurizes the capsular bag and the posterior capsule splits wide open from the force (figure 3). Now this cataract is in danger of falling into the vitreous due to the infusion pressure once the phaco probe is placed in the anterior chamber.
This case can still be saved, by bringing the nucleus up, out of the capsular bag. It can be brought up using a chopper or other second instrument, then additional viscoelastic can be placed under the nucleus to provide further support and to prevent vitreous prolapse. The nucleus can then be removed using a scaffold technique or a scleral tunnel can be made for manual nucleus extraction. The main incision will then need to be closed and then a bimanual approach can be used for cortex removal and anterior vitrectomy. A three-piece IOL can be placed securely with the haptics in the sulcus and the optic captured through the capsulorhexis.
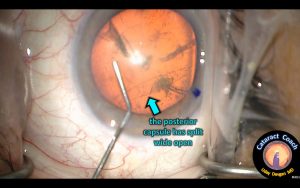
In the case shown here, the anonymous surgeon did not perform these techniques because the capsule defect was not recognized ahead of time. When the surgeon placed the phaco probe in the eye and attempted to sculpt the nucleus, the entire lens dropped into the vitreous cavity. The patient was referred to a vitreo-retinal surgeon who performed a pars plana vitrectomy and lensectomy and securely placed a sulcus IOL. Ultimately, the patient did well and recovered good vision.
With the high volume of intravitreal injections being performed every year, even a complication rate as low as 1 in 5000 means that 2000 patients per year will suffer a damaged lens capsule. This means that virtually every cataract surgeon will encounter this condition. Fortunately, we can spot this damage in most cases ahead of time and then take precautions to help ensure a good outcome for these patients.
Disclosures: Dr. Devgan owns CataractCoach.com which is a free teaching website. Visit CataractCoach.com
